
In the complex world of renal pathology, a kidney biopsy is often not enough to make a definitive diagnosis in certain patients. This is when diagnostic genetic testing can help. Genetic testing using next-generation sequencing (NGS; also known as high-throughput sequencing) is fast becoming a valuable tool for clinicians to help manage complicated cases and provide a personalized approach to patient treatment.
Washington University is fortunate to have Genomics and Pathology Services (GPS), which launched its first clinical NGS test nearly five years ago. Since then, GPS has been providing genomic testing for cancer, rare somatic diseases, severe congenital neutropenia and a variety of cardiac and renal diseases. The service also offers customized tests for clinical trials and clinical research.
Using NGS, coding exons of the targeted genes are sequenced to detect genetic variation at the level of a single nucleotide or small insertions and deletions. For constitutional disease testing, the GPS laboratory now uses the Clinical Research Exome (or Medical exome) assay, which has improved coverage of ~4600 medically-relevant genes known to be associated with human genetic diseases. Through bioinformatic processing, only genes relevant to the patient disease are analyzed, and the corresponding sequence changes (variants) are classified in relation to pathogenicity in the clinical report. The congenital neutropenia, cardiovascular disease and renal disease gene sets are actually all discrete subsets analyzed from the larger medical exome assay.
Benefits of exome-based testing. The type of testing performed at GPS is advantageous in that new or expanded gene sets can be launched relatively quickly, since the underlying exome reagent has already been through a rigorous validation phase. Consequently, as new, clinically relevant gene targets emerge in the scientific literature, GPS can nimbly respond to meet the needs of physicians and clinical investigators. All of the constitutional and cancer disease testing is accomplished through close collaboration with the treating physicians in various disciplines. In addition, in the research setting, the information obtained by sequencing the entire exome provides a valuable source of genetic data for analysis in IRB approved studies. Research in this setting lends promise to expanding the scientific knowledgebase surrounding associations between specific genes and diseases.
Expanded Renal Gene Panel. GPS has recently expanded and restructured the renal disease-specific tests to make them more clinically useful for the ordering physician. Genomic testing for renal diseases includes the following:
- aHUS/TMA/C3 Glomerulopathy (13 genes: ADAMTS13, C3, CD46, CFB, CFH, CFHR1, CFHR2, CFHR3, CFHR4, CFHR5, CFI, DGKE and THBD).
- Alport Syndrome (3 genes: COL4A3, COL4A4 and COL4A5)
- Nephrotic Syndrome and Focal Segmental Glomerulosclerosis Gene Set (34 genes: ACTN4, ADCK4 (COQ8B), ANLN, APOL1, ARHGAP24, ARHGDIA, CD2AP, COL4A3, COL4A4, COL4A5, COQ2, COQ6, CRB2, CUBN, EMP2, INF2, ITGA3, ITGB4, LAMB2, LMX1B, MEFV, MYH9, MYO1E, NEIL1, NPHS1, NPHS2, PDSS2, PLCE1, PTPRO, SCARB2, SMARCAL1, TRPC6, TTC21B and WT1)
- Cystic Disease and Nephronopthisis – New Test Offering (23 genes: AHI1, CEP290, GLIS2, INVS, IQCB1, NEK8, NPHP1, NPHP3, NPHP4, RPGRIP1L, TMEM67, TTC21B, XPNPEP3, BICC1, CRB2, EYA1, HNF1B,PAX2, PKD1, PKD2, PKHD1, SIX5 and UMOD)
Sequencing results, obtained from a simple blood sample, are accompanied by concise, expert interpretations by board-certified clinical genomicists. Turnaround time for the results is four to six weeks.
Genetic testing can not only help definitively diagnose a certain disease, it can also predict the likelihood of certain diseases developing, even in presymptomatic patients, and aids in the process of making informed decisions about medical treatment. With the development of NGS technology, genetic testing has become more accessible. Approximately 100 requests for renal genetic testing at GPS were made in the past year.

Jonathan Heusel, MD, PhD, GPS Chief Medical Officer
Will NGS replace biopsies? When asked if genetic testing will replace renal biopsies, GPS Chief Medical Officer Jonathan Heusel, MD, PhD, says, “No – the hallmark of genetic renal disease is one of incomplete penetrance and variable expressivity, so having a mutation does not necessarily mean there is underlying disease in the kidneys. Biopsies remain a critical component of the diagnostic and prognostic process. In addition, we still do not understand a great deal of the genetic causes for renal disease, especially the modulating variants and polymorphisms that affect disease penetrance and expressivity.” In essence, not all renal diseases are caused by genetic variation and not all individuals harboring such variants will develop renal disease, therefore pathologic review of biopsies remains a critical component of the diagnostic and prognostic process.
Why request NGS in the context of renal disease? The most frequent “typical” reasons for requesting genetic analysis are:
- To confirm a diagnosis – there are relatively few renal disease where the absence of mutation in defined gene(s) could formally rule out a diagnosis
- To evaluate prognosis – how quickly is the disease likely to progress; are there other syndromic manifestations to be aware of; what are anticipated therapeutic needs; will additional testing be needed?
- Drug and other treatment selection – as an example, the effectiveness of the monoclonal antibody eculizamab has been established for diseases of inappropriate complement activation/regulation such as aHUS;
- To establish carrier status and family screening/planning
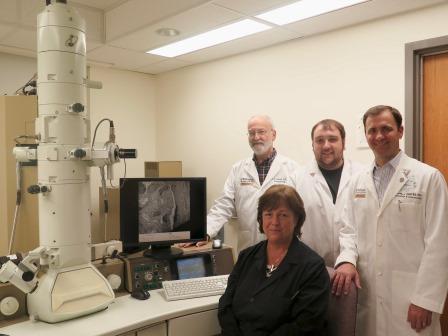
(Back, L-R) Robert Schmidt, MD, PhD; Christopher Dunham; Joseph Gaut, MD, PhD; (Front) Karen Green.
Genomic testing just part of the services offered. Dr. Heusel points out that the genetic testing offered by GPS is just a part of a greater whole comprised of the integrated pathology and molecular testing services offered by the Pathology & Immunology Department. In fact, Washington University Diagnostic Laboratory Services, the clinical arm of the Department of Pathology & Immunology, now offers full-service renal biopsy testing to outside hospitals in addition to handling internal cases. Every kidney biopsy gets a comprehensive work-up including routine examination by light and transmission electron microscopy, as well as the use of immunofluorescence and a variety of special stains. Robert Schmidt, MD, PhD, Head of the Division of Neuropathology and Director of the Electron Microscopy Facility, says that it is not just the hi-tech equipment that makes this a state-of-the-art EM facility … it is the expertise of the team that makes the facility stand out. Making up the team is: Joseph Gaut, MD, PhD, Assistant Professor, Pathology & Immunology and Medicine, a subspecialty expert in renal pathology; Karen Green, technical Director-Research EM Facility, who can boast of over 40 years of experience in electron microscopy (18+ in kidney biopsy analysis); and hard-working technician Christopher Dunham who joined the team four years ago. “Put it all together, we have really proved that is what makes this [facility] special,” Dr. Schmidt emphasized.
Physicians interested in kidney genetic testing for their patients may contact GPS by phone at 314-747-7337 (toll-free 866-450-7697), email at gps@wustl.edu or visit their website.