Overview
The Nephrology Transplant Fellowship is one of the most comprehensive training programs of its kind in the country. We emphasize both teaching and scholarship in a vibrant and high-volume setting that provides trainees with multiple opportunities for inpatient and outpatient care, as well as HLA lab, transplant pathology, research and other scholarly activities.
We accept two transplant fellows and one possible research fellow annually. Our program has sufficient volume to allow for maximal exposure to a wide variety of patient encounters. Each fellow will experience every aspect of renal and pancreas transplantation first hand. Our program structure provides ample time during off-service months to work on research projects. We have a scheduled weekly transplant specific didactic, as well as regularly scheduled combined transplant grand rounds. Throughout the fellowship, trainees are encouraged to read and present relevant articles in transplant to expand their knowledge of the field.

Program highlights
The Washington University Barnes-Jewish Transplant Center is one of the largest and most experienced center in the United States. The center celebrated its 10,000th transplanted organ in 2019. The Division of Nephrology is consistently ranked among the nation’s best by U.S. News & World Report for the treatment of kidney diseases.
We offer transplant fellows:
Training in a large tertiary center – Our base hospital is Barnes-Jewish hospital, a 1,300-bed hospital with a large catchment area. This provides the transplant fellow a large breath of patient care interactions throughout the year such that the fellow will feel comfortable caring for even the most complex patients upon graduation.
High transplant volume —We perform more than 325 kidney and 15 kidney-pancreas/pancreas transplants annually. About 30 percent of all kidney transplants are with living donor transplants. This is sufficient volume for fellows to meet UNOS requirements to be kidney/kidney-pancreas program directors.
Nationally recognized, experienced faculty — Kidney transplant survival rates, which continually remain better than national averages, are a reflection of the program’s expertise. Our acute rejection rate following a kidney transplant is less than 7 percent at one year, one of the lowest kidney transplant rejection rates in the world. We have an ABO incompatible transplant program and are actively involved in paired kidney exchange programs for recipient/donor pairs who are difficult to match. We also have a burgeoning Hepatitis C positive donor into Hepatitis C negative recipient program as well as HIV positive recipient program.
Multidisciplinary practice opportunities — We offer a wide variety of inpatient and outpatient clinical opportunities for our transplant fellows. The rotations are split, with 6 months of inpatient services, 4 months outpatient clinic, 1 month HLA lab and elective rotation, and 1 month vacation. When doing outpatient clinic, the fellow has 4 half days a week without clinical duties.
An intensive HLA course and deep exposure to HLA medicine are offered under the supervision of Chang Liu, MD, PhD, and Donna Phelan. Please visit the HLA Lab for more information.
Based on the number of biopsies, there is a weekly or twice weekly review session(s) with Nidia Messias, MD, or Joseph Gaut, MD, PhD. Dr. Gaut is famous for his YouTube nephrology educational series with Tim Yau, MD.
- Inpatient: We have a strong relationship with our transplant surgical colleagues. Inpatient rounds include medical and surgical consultants, residents, physician assistants, nurse practitioners, transplant pharmacists, and nurses. Fellows lead rounds and participate in all aspects of inpatient care under close supervision by the attending. In addition to the transplant nephrology fellow, there is a general nephrology fellow and a nurse practitioner. The service includes the management of new transplants, pending transplants and patients with previous transplants who have new renal complications. This service also provides in-patient consultations for acute kidney issues in patients with other solid organ transplants including liver, heart and lung.
- Outpatient: Fellows evaluate patients as potential kidney or pancreas transplant recipients as well as evaluate possible living donors. Fellows also actively participate in the short-term and long-term care of transplant recipients. We have a deep commitment to our patient population and follow them throughout the life of their allograft. Fellows also attend the weekly kidney transplant selection conference, weekly patient review meeting, and weekly living donor conference.
Research opportunities — Washington University scientists are known worldwide for their ongoing development and refinement of immunosuppressive therapy to prevent rejection, as well as strategies to prevent infection. Some of the seminal contributions resulting from work done at Washington University include: research on the use of rabbit anti-thymocyte globulin given intraoperatively for induction therapy; the evaluation of prophylaxis and pre-emptive strategies for CMV prevention post-transplant; and treatment of BK viral infection and prevention of nephropathy through medication reduction. Fellows are expected to join other transplant nephrologists’ research projects that are funded both intramurally and extramurally. Fellows will have time during the outpatient setting to initiate, perform and publish an article.
Educational conferences — Multiple opportunities for vibrant, didactic discussions occur in daily and weekly conferences. Weekly conferences include the Journal Club and Case Conference, Transplant Selection Conference and Renal Ground Rounds. The Division of Nephrology also has a daily conference at noon. A combined transplant Grand Rounds occurs monthly, where different speakers from all specialties within solid organ transplant are invited to discuss innovative projects and new discoveries in transplantation.
Midwest Transplant Symposium — This is an annual symposium that offers hands-on workshops on HLA, ultrasound, and transplant pathology. In addition, speakers from around the United States are invited to present their work.
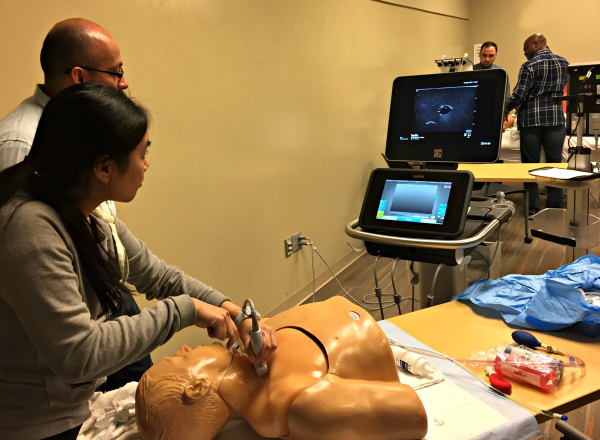

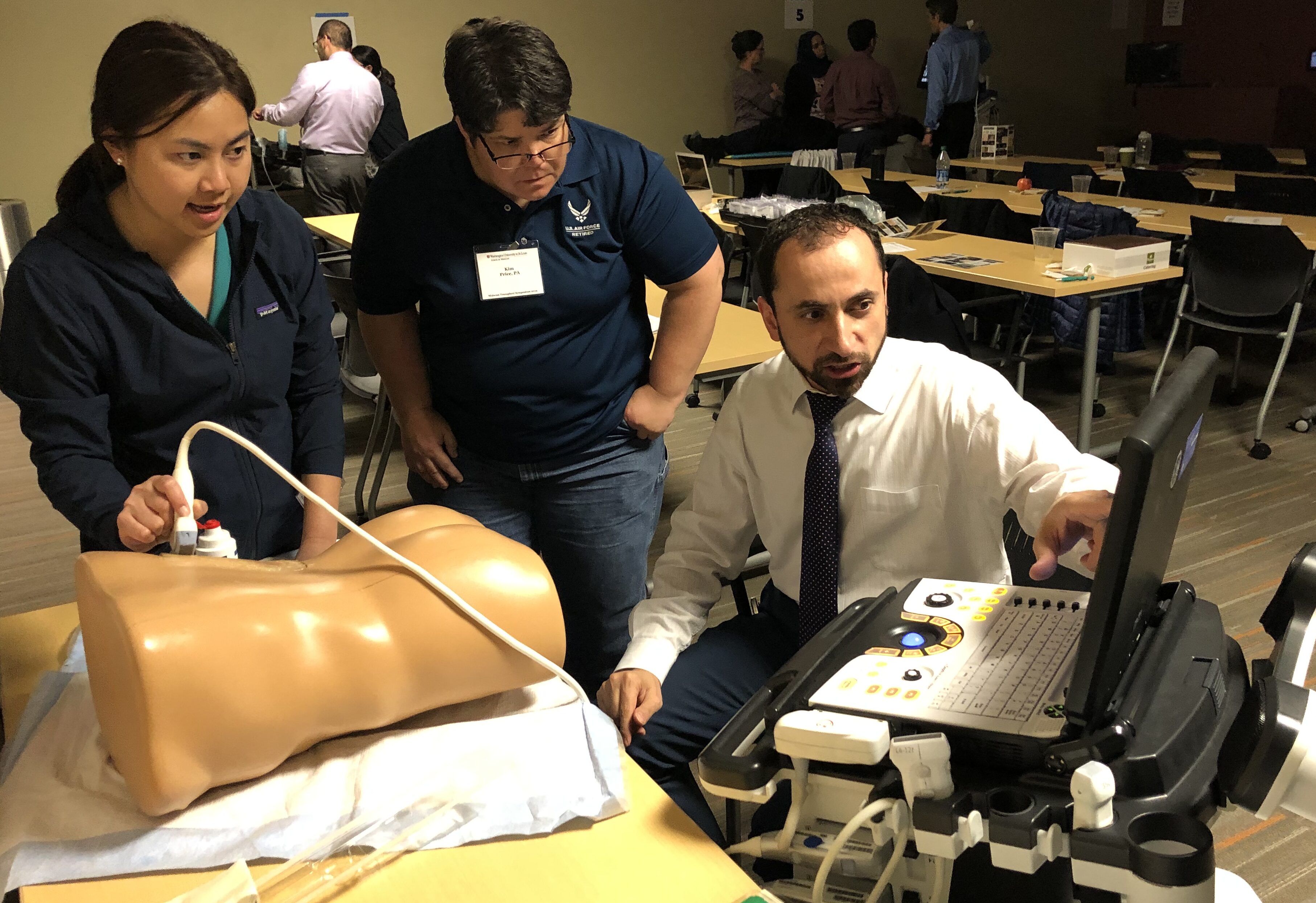
Midwest Transplant Symposium, 2019
Transplant fellowship faculty & staff

Tarek Alhamad MD, MS, FACP
Medical Director, Transplant Nephrology
Professor of Medicine
X: @TransplantPulse

Massini Merzkani, MD
Director, Nephrology Transplant Fellowship
Assistant Professor of Medicine
X: @massini_me

Anuja Java, MD
Director, Kidney Transplant Clinic at Veterans Affairs St. Louis Health Care System
Associate Professor of Medicine
X: @anuja_java
Read About Our Current Transplant Fellows Here

Transplant fellowship application process
The transplant fellowship is geared to applicants who have completed an AGGME-accredited nephrology training program. We offer J1 and H1 VISA support. Internal Medicine Residency outside the US is acceptable for selected candidates.
Complete the Transplant Fellowship Application (pdf) and follow directions to mail or email the form to our program.
If you have questions about our Transplant fellowship program, please contact:
Laura Kipper
Fellowship Program Coordinator
Washington University School of Medicine
660 S. Euclid Ave., Campus Box 8126
St. Louis, MO 63110
Phone: 314-362-8351
lkipper@wustl.edu
Massini Merzkani, MD
Assistant Professor of Medicine
Director, Transplant Nephrology Fellowship
Washington University School of Medicine
660 S. Euclid Ave., Campus Box 8126
St. Louis, MO 63110
massini@wustl.edu
The 2019 ASN TV video below highlights our transplantation and home modalities programs.



