Faculty and fellows sporting WashU #nephSTRONG t-shirts.
2020 will certainly be a year our fellows will remember.
The WashU Nephrology fellowship training program provides a strong clinical training and research experience for our fellows during their time with us. The fellows see patients in Barnes-Jewish Hospital (including the ICUs), attend to patients undergoing dialysis at Chromalloy Kidney Center, monitor the home modalities patients at Forest Park Dialysis Center, and care for patients in our various clinics in the Center for Advanced Medicine. They do all of this in addition to studying for their boards, completing their research projects, and performing other scholarly activities.
Top all of that off with a pandemic, and you have one memorable year.
Kept in the Loop

Dr. Frank O’Brien, associate program director for curriculum development, Nephrology Training Program.
“COVID-19 started to become a regular part of both faculty and fellow life by mid-March of this year,” says Frank O’Brien, MBBCh, MRCPI, associate program director for curriculum development, Nephrology Training Program. “There were huge changes happening throughout the University and hospital aimed at dealing with the pandemic. At that time, we agreed to suspend educational conferences for a time to allow for social distancing and to allow fellows and faculty to adapt to these new changes.” In addition, to protect the fellows, the faculty created an attending-only service for COVID-19 positive patients.
“It seemed at that time things were changing hourly and, naturally, stress levels started to rise,” says O’Brien. To combat this, the training program leadership team initiated new practices and procedures, starting with increased communication to keep the fellows informed as to what was going on both in the division and in the hospital.

Dr. Seth Goldberg, associate program director for service and assessment, Nephrology Training Program.
“We have been proactive in maintaining a steady line of communication with the fellows, which serves to keep spirits up and ease uncertainty,” says Seth Goldberg, MD, associate program director for service and assessment, Nephrology Training Program. “Our daily email updates review the hospital census numbers for COVID-19 positive patients, the number of available ICU beds and ventilators, and the number of dialysis machines in use and in reserve.” Goldberg believes that keeping the fellows informed of the steps our institution has taken to prepare for a potential surge allows them to know precisely where we stand with regards to the progression of the pandemic as well as availability of resources.
Digital Life
Like everyone else, the fellows feel the stress of these strange times and the limitations it has created. Clinics are now conducted almost entirely remotely, either by telephone, or preferably through a video interface, mainly with Zoom. “There are actually some very real benefits of conducting the clinics this way, aside from the social distancing it provides,” says Goldberg. “There is less downtime between patients, allowing for more direct physician-patient interaction, it saves travel time for patients who live who do not live in the St. Louis area, and there is lower risk of “no-shows” or patients getting in late due to traffic or parking. We anticipate that some degree of tele-medicine will become a permanent part of our practice even after the COVID restrictions resolve.”
“We also instituted a weekly Zoom ‘check in’ fellows meeting to ensure everybody felt connected while socially distancing,” says O’Brien. The informal meeting gives everyone the opportunity to ask and answer questions that may arise. In addition, On Thursday evenings, there is weekly town hall-style meeting with the Internal Medicine chair for the fellows with all divisions invited.
A Sense of Comradery
Dr. Tingting Li, associate program director for clinical research & career development and wellness, Nephrology Training Program.
Tingting Li, MD, MSCI, associate program director for clinical research & career development and wellness, Nephrology Training Program, says, “This is a challenging time for everyone, but particularly for the trainees. There was understandably fear and anxiety in the beginning, but our fellows have really stepped up. They continued with their regular patient care activities while supporting each other and the division.”
Li points out that the fellows eagerly pitched in to cover the clinical service when one fellow was quarantined and bravely applied for disaster privileges, ready to be deployed to areas of need in the hospital. The fellows also learned to effectively allocate resources such as dialysis machines, communicated daily with the acute dialysis nurse to coordinate dialysis care, and transitioned smoothly from normal clinic visits to telehealth clinics.
“The leadership team also ensures that the on-service fellows are provided weekly lunches,” says Li. “The lunches and the weekly Zoom chats help the fellows debrief and boost morale.” O’Brien also believes that this sense of comradery is important for everyone involved, “This ensures that as a group, we can all support each other through what was – and still is – a very trying time.”
“We really appreciate the fellows’ hard work, their ability to adapt to the new normal, and their positive attitude,” says Li. “We are proud of them.”

Faculty and fellows enjoy LaCroix water donated by the National Beverage Corporation.
Forging Ahead
Despite this difficult time, the fellowship continues to be committed to the mission of clinical training, education, and research.
“As we adapted to the new normal, we started to re-introduce educational activities on a phased basis,” says O’Brien. “We started with weekly board-review Q&A sessions, led by professor of medicine, Dr. Aubrey Morrison, MBBS, MACP, FASN, via Zoom. These proved successful, and have since fully restored all educational activity, including fellows grand rounds. It has seemed strange to conduct all teaching through video conference, but our fellows have adapted quickly and are now Zoom experts!”
Goldberg agrees. “The conferences have run extremely smoothly, with a high level of fellow participation and back-and-forth interaction. It is yet another component which may persist after the passage of COVID.”
Regarding their research, Li says, “The fellows are actively engaged in their research projects and are getting ready to present their data to the division in the coming weeks. In addition to her own ongoing research project, second-year fellow Christina Mariyam Joy, MD, volunteered to be part of the WashU research team for a multi-center COVID-Acute Kidney Injury study and contributed significantly to the data collection.”
As well, the fellows have kept up with their studies. Sam Krishnamoorthy, MBBS, our transplant fellow, has been giving a series of transplant lectures to the general nephrology fellows via Zoom, and in addition to the board Q&A with Dr. Morrison, various faculty have been presenting pathophysiology lectures.
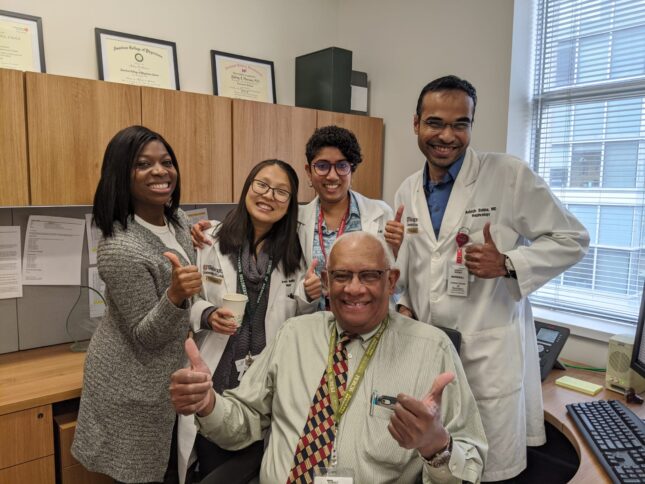
Dr. Aubrey Morrison (seated) spends time with some of the fellows pre-COVID! (From left: Drs. Blessing Osondu, Irene Nunuk, Madhuri Ramakrishnan and Aniesh Bobba.)
Here are our fellows:
Second-year fellows
 Aniesh Bobba, MD
Aniesh Bobba, MD
“These were indeed stressful times. I appreciate our program leadership’s hard work and commitment toward trainees. We were always kept in the loop with constant communication and multiple strategies were implemented to help us get through. To mention a few COVID 19 attending service, daily email updates on COVID 19, Wednesday lunch, Thursday zoom fellows wellness conference, delivery PPE supplies directly to the fellows. It clearly showed us “We care about you and here to help.” That’s all we need to know to get through this period.
Follow on Twitter @anieshb

Andy Chuu, MD
“I am very grateful for the tremendous effort and coordination that our program and divisional leadership has taken in response to the COVID19 pandemic. They have focused their efforts on fellow safety by providing additional PPE (some of which were obtained by faculty personal funds) and minimizing fellow exposure to COVID19 with the creation of a COVID attending only service. In addition to their response in fellow safety and patient care, they have also made great efforts to maintain important aspects of fellow training, such as education and wellbeing. I appreciate all that has been done by the faculty within our division to support the fellows and am also inspired by their efforts in battling this pandemic.
“We are all in this together! #nephSTRONG!” Follow on Twitter @ChuuAndy
 Christina Mariyam Joy, MD
Christina Mariyam Joy, MD
Follow on Twitter @JoyMariyam.

Irene Nunuk, MD
Follow on Twitter @irene_nunuk
 Madhuri Ramakrishnan, MD
Madhuri Ramakrishnan, MD
“Nothing reveals the true nature or ability of your tribe than a crisis situation. The way the division of nephrology has banded together for both the patients and the fellows is not just commendable, but aspirational for us trainees”
Follow on Twitter @madmagicdoc
First-year fellows
Reena Gurung, MD

Gonzalo Matzumura, MD
“I think there was a lot of uncertainty and anxiety at the beginning when we started realizing the magnitude and the impact the pandemic would have on our daily lives and training. However, I am very grateful and relieved that our leadership proactively stepped-up to ensure our safety and our training. They kept us informed every step of the way and made extra efforts to check-in on us and make sure we were doing well. I am actually excited that some new activities that were adopted out of necessity in this crisis (e.g., interdisciplinary conferences, board review sessions and telemedicine visits) might become fixtures going forward.”
Follow on Twitter @GMatzumura
 Maggie Meier, MD
Maggie Meier, MD
 Blessing Osondu, MD
Blessing Osondu, MD
“The COVID-19 pandemic has definitely been a memorable time for me. I am grateful, however, that it happened during my nephrology fellowship at Washington University. Not only do we have supportive leadership, I have my colleagues to rely on during this stressful season. I am able to pick up my phone at any time during the day to talk with a few of my colleagues, and in each other we find strength. We receive text messages, emails, lunch, PPEs and most of all, our education has not been compromised in any way.
I am not alone; you are not alone; we are not alone. Together we will prevail!!!”

Sana Javeed Shaikh, MD
Follow on Twitter @always_oncall

