The 3rd Midwest Nephrology & Transplant Symposium Ultrasound Workshop, held September 8-10, 2017, at Washington University School of Medicine, was a success.

Tarek Alhamad, MD
“Turnout was excellent,” says Dr. Tarek Alhamad, Assistant Professor of Medicine in Transplant Nephrology and the symposium’s Course Chair. “For the Ultrasound Workshop, we reached a maximum of 25 participants, with 6 instructors.” The instructors, there to provide comprehensive training, were from the critical care divisions of Emergency Medicine, Surgery, and Anesthesiology.
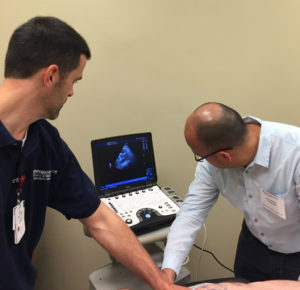
 The Ultrasound Workshop, directed by Dr. Enyo Ablordeppey, Assistant Professor in Anesthesiology and Emergency Medicine, was a new feature of the symposium this year. The intensive training course allowed participants to build skills in the examination of heart, lung, renal, and inferior vena cava volume assessment, as well as ultrasound-guided techniques for vascular access and renal biopsy. The workshop had hands-on ultrasound scanning with human models, case didactics, ultrasound diagnostics, and procedural simulation.
The Ultrasound Workshop, directed by Dr. Enyo Ablordeppey, Assistant Professor in Anesthesiology and Emergency Medicine, was a new feature of the symposium this year. The intensive training course allowed participants to build skills in the examination of heart, lung, renal, and inferior vena cava volume assessment, as well as ultrasound-guided techniques for vascular access and renal biopsy. The workshop had hands-on ultrasound scanning with human models, case didactics, ultrasound diagnostics, and procedural simulation.
 “Participants really seemed to enjoy the course and provided very positive feedback,” says Dr. Ablordeppey. “The workshop was a great start. Clinical providers will now have to go to the patient’s bedside to improve their skills with ultrasound.”
“Participants really seemed to enjoy the course and provided very positive feedback,” says Dr. Ablordeppey. “The workshop was a great start. Clinical providers will now have to go to the patient’s bedside to improve their skills with ultrasound.”
Testing at or near the site of patient care is referred to as point-of-care testing, which not only allows for more rapid therapeutic action, but is considered a more efficient use of healthcare resources. When performed with ultrasound, the testing is referred to as point-of-care ultrasound, or POCUS.
“POCUS of cardiac, lung, and inferior vena cava diameter and collapsibility have emerged as useful tools in volume assessment,” says Alhamad. “The ultrasound volume assessment has been underutilized in the care of our kidney disease patients in the floor, intensive care unit, and in hemodialysis centers.”
“POCUS plays a crucial role in patient care by allowing the clinician to immediately integrate the physical exam and acquire images to determine patient physiology and guide management,” notes Ablordeppey.
Programs like the ultrasound workshop will continue to highlight the importance of POCUS in patient hemodynamic volume assessment and procedural guidance.
“We are looking forward to expand the program next year to have a full day as POCUS and another day focusing on renal ultrasound,” says Alhamad, already planning the next workshop!